Is it still “time to choose”? How patient choice can enable NHS patients to access faster care
Introduction
In 2022, IHPN published a report with the Patients Association “Time to Choose” which looked at how patients exercising their right to choose can help clear the NHS elective backlog. It found that across England, patients needed to travel just 13.2 miles – around 30 minutes by car – to cut over three and a half months off their waiting time, moving from providers with an average of 22 weeks to an average of just 8 weeks.
These included some specific regional disparities, particularly in the South West where the difference between the providers with the best and worst waits was over 18 weeks (four months). General surgery patients, for example, in the South West waiting in the bottom third of providers currently were waiting on average over 35 weeks for treatment. This compares with patients waiting in the top third of providers who were waiting on average just 9 weeks – a disparity of over 26 weeks (6 months).
Two years on, and with welcome cross-party consensus around the importance of patient choice, we were keen to understand the variations in waiting times across the country and if it’s still possible for patients to access faster care by choosing an alternative provider in their region.
Key findings
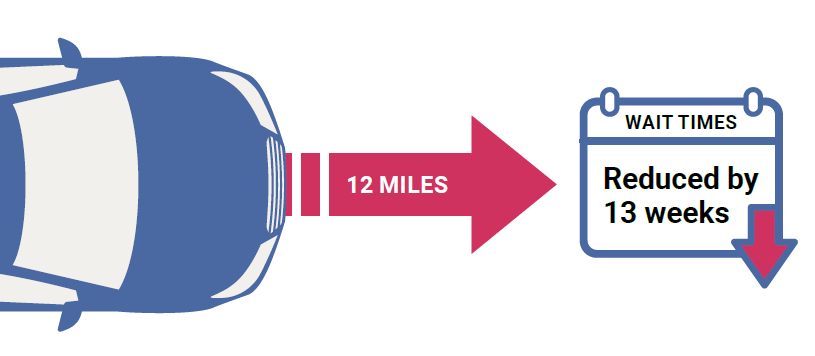
Overall, our analysis of NHS waiting times across the country found that patients in England can cut months off their wait for care by exercising their right to choose a different provider for their NHS treatment. Across England, patients need to travel on average just 12 miles – typically under 25 minutes by car – to cut 3 months off their waiting time.
Looking at the data in more detail, there are significant variations in NHS waiting times across both regions and specialties, with the opportunities for patients to access much faster care.
The disparities can be seen clearly in the North West, where the difference between the providers with the best and worst waits is over 14 weeks (3.5 months). Looking at individual specialties in the North West, urology patients waiting in the bottom third of providers currently wait on average 24 weeks for treatment. This compares with patients waiting in the top third of providers who wait on average less than 8 weeks – a disparity of 16 weeks (4 months).
Looking at individual specialities, there are significant differences in waiting times in each region.
Trauma and orthopaedics
Patients waiting for trauma and orthopaedics treatment in the bottom 1/3 of providers in the South West wait on average 23 weeks, while patients waiting in the top 1/3 of provider wait just over 9 weeks – a disparity of 14 weeks (3.5 months).
Likewise in the South East, patients waiting in the bottom 1/3 of providers wait on average 19 weeks, while patients waiting in the top 1/3 of provider wait just under 7 weeks – a disparity of over 12 weeks (3 months).
General Surgery
Patients waiting for general surgery in the bottom 1/3 of providers in London wait on average almost 21 weeks, while patients in the top 1/3 of providers wait just under 7 weeks – a disparity of over 14 weeks (3 months).
In the East of England, patients waiting for general surgery in the bottom 1/3 of providers wait on average almost 21 weeks, while patients in the top 1/3 of providers wait just under 8 weeks – a disparity of over 13 weeks (3 months).
Ear, Nose and Throat
There are significant disparities in waiting times for Ear, Nose and Throat patients. Those waiting in the bottom 1/3 of providers in the South East wait on average almost 36 weeks, while patients in the top 1/3 of providers wait just under 7 weeks – a disparity of over 29 weeks (6 months).
Likewise in the North East and Yorkshire, those waiting in the bottom 1/3 of providers wait on average almost 22 weeks, while patients in the top 1/3 of providers wait around 9 weeks – a disparity of over 13 weeks (3 months).
Urology
Waits for urology care in the North West vary from over 24 weeks for the bottom third of providers, down to just over 7 weeks in the top third – a range of almost 17 weeks.
Ophthalmology
Waits for ophthalmic care in the East of England vary from over 17 weeks for the bottom third of providers, down to just over 3 weeks in the top third – a range of over 14 weeks.
Gynaecology
Waits for gynaecology care in the North West vary from 23.5 weeks for the bottom third of providers, down to just over 10.9 weeks in the top third – a range of over 12 weeks.
How far do patients need to travel to access faster care?
As part of our analysis of waiting times, we also looked at how far a patient waiting in the worst performing third of providers would have to travel to get faster care in the top third of providers. Overall, our analysis has found that across the country, the average distance a patient would need to travel to move from a provider with one of the longest waits to a provider with one of the shortest waits is just 12 miles – or less than 25 minute drive. Doing so would potentially translate to saving 13 weeks’ waiting by moving from providers with an average of 20 weeks to an average of 7 weeks.
Looking at this on a regional level this means that, in the Midlands for example, a patient waiting for treatment in one of the third lowest performing providers would need to travel an average of just 11.8 miles to one of the top third of providers to see their average waiting time go from 20 weeks down to 8.5 weeks – a saving of almost 11.5 weeks.
In the North West you would need to travel just 8.5 miles to see your waiting times cut by an average of over 16 weeks from 21.3 weeks to 14.3 weeks.
What do the public think about patient choice?
We commissioned polling from Savanta ComRes on the public’s current awareness and attitudes to patient choice, as well as their willingness to travel to receive faster care.
Overall, a slim majority (55%) said they knew that there was a legal right to choose a hospital or clinic for a first NHS outpatient appointment. This reduced to 50% who were aware of their legal right to change hospital if they had to wait more than 18 weeks before starting NHS treatment, and just 44% who were aware of their legal right to choose who carries out a specialist NHS test. Just 40% of the public knew that they can choose to receive their first NHS outpatient appointment in an independent/private sector provider with no additional cost to the NHS.
The polling overall showed that the public are, however, enthusiastic about patient choice. Almost three quarters (73%) of people believe they “should have a right to choose where I receive my NHS treatment, including with an independent/private sector provider”. This rises to over eight in ten people (81%) agreeing that they are happy to receive NHS care with an independent/private sector provider as long as they are subject to the same quality standards as the NHS and it costs the standard NHS price.
Overall, the polling also found that people are comfortable with travelling outside their local area to receive their NHS care. Over seven in ten (71%) people reported being happy to travel more than 30 mins outside of their local area to get faster treatment. Only 5% of people said they would not travel outside their local area to get quicker treatment from the NHS.
This willingness to travel for treatment emphasises the importance of empowering patients with knowledge on their choice of providers. Our analysis shows, for example, that 96% of people in England live within 30 minutes driving distance of an independent provider that delivers NHS treatment. For those that are less able to travel independently, NHS have introduced measures to support travel and accommodation needs to help improve equality of access to these treatment options.
When asked about any potential barriers to accessing NHS treatment outside of their local area, the polling found their biggest concern was around the cost of travel (27%), followed by where follow-up care would be available (identified by 22%).
Methodology
IHPN have analysed NHS RTT performance data for March 2024, published in May 2024, looking specifically at median waiting time for incomplete pathways, i.e. how long people have on average waited so far who are yet to begin substantive treatment.
As part of this analysis we have looked at the NHS’ top six treatment functions – trauma and orthopaedics; ophthalmology, ear nose and throat, gynaecology, general surgery and urology (NB we excluded “other” treatments from this list because while they make up some of the largest treatment groups, it is a very broad and ill-defined category)
To make meaningful comparisons between providers we have identified the top and bottom third of providers by median waiting times.
For each specialty and region, we have looked at all non-specialist providers with waiting list above a minimum threshold of five people, whilst also excluding organisations that may have atypically short waiting lists because they are, for instance, part of cancer pathways.