
NHS productivity – does ophthalmology have an answer?
18/12/2023
David Hare writes how ophthalmology’s 15 per cent activity boost and reduced wait times exemplify NHS productivity, with the independent sector delivering 160 per cent more care, emphasising the potential for specialisation and patient flow improvements as vital lessons for broader health system gains
When the chancellor, Jeremy Hunt, stood up to deliver his autumn statement in November, there was one thing on his mind seemingly more than any other – “productivity”. With seven mentions in his speech and 42 in the supporting papers, productivity is clearly the focus nowhere more so than in the public sector, specifically the NHS.
There’s a “Productivity Review” reportedly on the way to NHS England, led by McKinsey, and Amanda Pritchard was quizzed at length on the topic at a recent Health and Social Care Select committee hearing.
With a waiting list growing year-on-year for a decade, dramatically exacerbated by the pandemic, a massive expansion in activity is needed to start tackling the elective backlog.
And, despite some tricky public finances, the NHS has had money to invest in its post-pandemic recovery.
According to the Institute for Fiscal Studies, the NHS employed 16 per cent more consultants in 2023 than in 2019, 25 per cent more junior doctors and 20 per cent more nurses and health visitors. Yet activity hasn’t followed. Emergency admissions are down 4 per cent, non-emergency admissions are down 1 per cent, outpatient appointments are up just 2 per cent and treatment from the waiting list is up 1 per cent.
Doctors, nurses, health visitors and other staff are working flat out. So why isn’t activity flowing better? Where is the productivity gap? Can the NHS realise its own productivity targets of 1.5-2 per cent, included in the long term workforce plan?
There are several obvious barriers – a lack of funding for capital investment and infrastructure, technology that doesn’t meet modern needs, and an ever-more challenging position for social care and the knock-on impact that has on patient discharge, to name but a few.
A change in approach – or, perhaps, a willingness to embrace (or at least consider!), other delivery models – is clearly needed.
We’ve seen it to some extent in diagnostics, where, at least partly thanks to the success of the Community Diagnostic Centre model, diagnostic testing is up more than 10 per cent in 2023 compared with 2019.
But perhaps the real success story of the elective recovery programme so far has been ophthalmology.
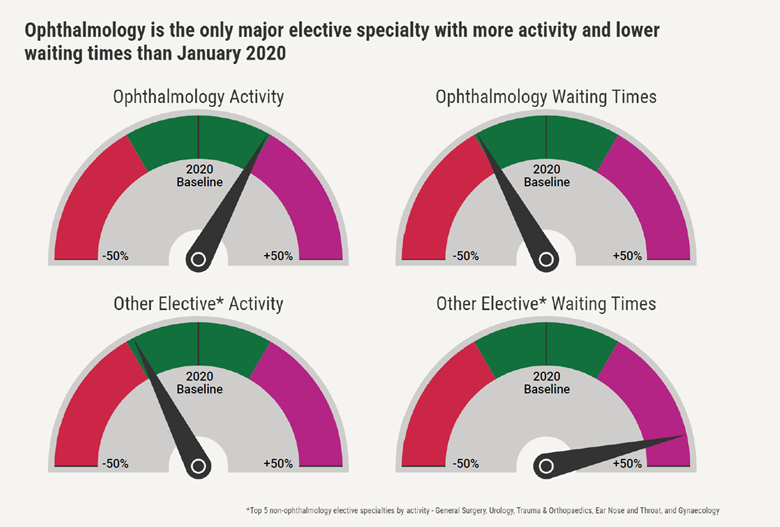
In ophthalmology, total activity is up more than 15 per cent in 2023 as compared to 2019 – and average waits are down by as much as two weeks.
This might seem modest, but put it in context: combined activity across the other top elective specialties by volume remains 15 per cent below pre-pandemic levels, and waiting times are up 43 per cent – an additional 9 weeks wait, on average, in the case of trauma and orthopaedics, for example.
So why is opthamology doing so much better?
A major factor is the role of the independent sector.
Compared with 2019, the independent sector is delivering 160 per cent more activity in ophthalmology. In 2023, the sector is projected to provide care for 440,000 NHS patients, with waiting times an average of just six weeks.
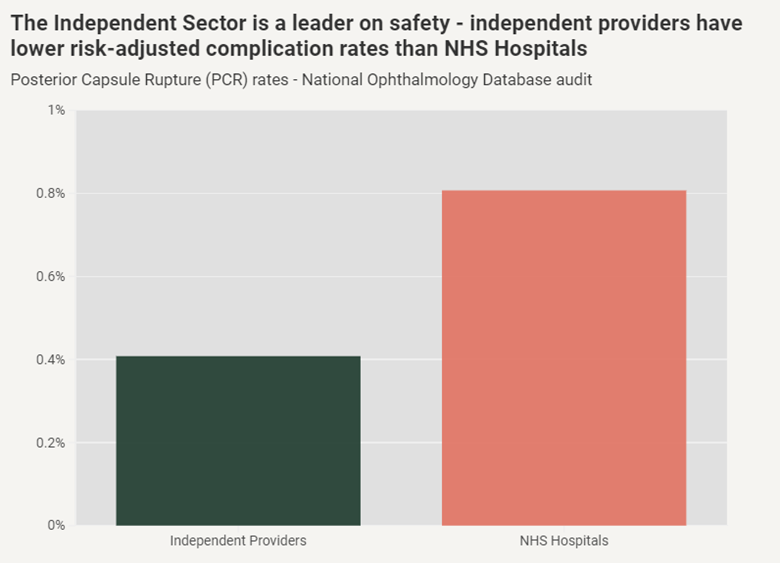
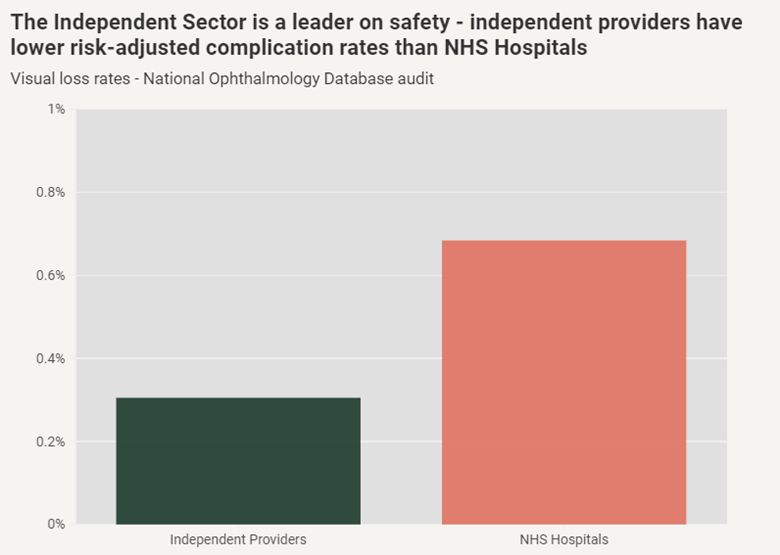
Crucially, the sector has maintained safety standards while it has done so. The National Ophthalmology Database audit showed that risk-adjusted complication rates are approximately 50 per cent lower at independent providers than in NHS hospitals.
One of the major lessons from ophthalmology is that the flow of patients is everything.
Referrals through the electronic referral system show where patient choice is working properly. Ophthalmology eRS referrals are up 130 per cent compared with 2019 – but total referrals across all other specialties remain 10 per cent lower than pre-pandemic.
We know some of the reasons why. High-street optometrists refer, via eRS, directly to independent providers. Patients can see their options, choose the providers with shorter lists and get the quickest possible access to treatment.
A second lesson – and perhaps the most important when it comes to productivity – is that specialisation breeds efficiency. The NHS knows this – it’s why there’s a programme of surgical hubs, and it’s why “high-volume, low-complexity” is a focus of the Getting It Right First Time programme.
So there’s lots which is positive. Activity is flowing, quality is excellent, more patients are being treated and waiting times are coming down.
But that’s not to say there aren’t challenges too, and it’s important we tackle them. Two points of concern at the moment we’ve heard are how we protect sustainable eyecare units at NHS trusts, and how we ensure that the future eyecare workforce is getting the right training and development.
We at IHPN, and our members, are committed to finding solutions here.
On training, there’s already good work happening. The sector is already training junior doctors, nurses, and a wide variety of other clinical staff – but providers can do more, and, they want to do more.
We’re working with NHSE and the Royal College of Ophthalmology to try and break down existing barriers and tackle the undoubted challenges which exist.
But, ophthalmology provision by the independent sector has been the biggest success story of the post-pandemic recovery to date.
The NHS should be embracing it, learning from it, and working with the sector – both to help shape the future of NHS eyecare and to understand how productivity gains can be replicated across the rest of the health system.
